African swine fever is a severe viral disease of pigs of all ages. In recent years it has devastated the swine industry in many different countries. ASF actually spreads rather slowly and it is possible to curtail its geographic spread by appropriate action. Early definitive diagnosis is a key element to avoid spread. An initial field diagnosis of African swine fever can be made from clinical signs and necropsy findings.
Clinical signs:

In the initial phase of the disease, animals are often found peracutely dead with cyanosis of the legs, ears, and the extremities. Often there is high fever 40 - 42° C, vomiting, diarrhea that may be bloody or black (Photo 1, right), depression, abortions (Photo 1, left), bloody nasal discharge (epistaxis), and increasing death losses.

The low virulence (vaccine) strains cause a mild chronic atypical form of the disease with few deaths. Females generally exhibit chronic respiratory disease and chronic infertility. The longer time course to obvious illness or lack of observed clinical signs among the chronic vaccine virus pigs is often interpreted by the farm as a long incubation period.
Lesions at necropsy
- Epiglottis and trachea may be reddened, and there is generally an interstitial pneumonia with inter-lobular edema. Sometimes there is a fibrinonecrotic pleuropneumonia that resembles APP.
- A fibrinous myocarditis and pericarditis may be present, and the thorax and abdomen may have an excessive amount of bloody or serosanguinous fluid.
- The mesenteric lymph nodes and particularly the gastro-hepatic nodes may be enlarged, edematous, and appear to be necro-hemorrhagic on the cut surface (Photo 2).
- The spleen may be enlarged with multiple infarcts present or it may be essentially normal.
- The liver often contains frank hemorrhages.
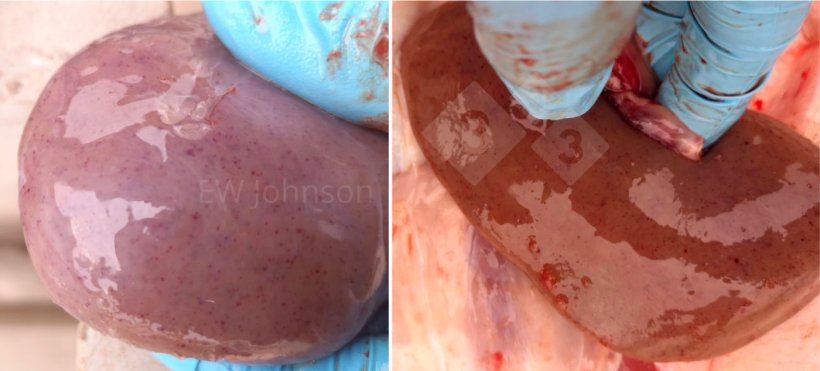
- The kidneys may have numerous infarcts, and petechial and ecchymotic hemorrhages (Photo 3). There may be a striking peri-renal edema. The fundic stomach is often severely reddened and eroded, and the spiral colon may be filled with a bloody content. It is not unusual to find paintbrush hemorrhages on the abdominal viscera.
- A fibrinous meningitis may be evident in the brain.

Necropsy should be done with a professional concern for biosafety, but necropsy does not introduce unique disease hazards to an infected farm and does provide valuable information not attainable by less aggressive diagnostic approaches.
Laboratory techniques
PCR: The diagnosis of ASF is usually verified by a positive nucleic acid test and by the ruling out of other common causes of similar lesions. The most common is PCR for the P72 gene. Lung (preferred sample in our lab), kidney, spleen, lymph node, serum, and blood are all excellent test samples for PCR. Oral swabs and oral fluids are extremely popular but the amount of virus is several logs less than what is generally found in blood and tissue, so false-negative results are rather common. Fluorescent qPCR and conventional PCR are employed for testing. Conventional PCR offers a convenient route to gene sequencing.
Where the gene deleted vaccine has been used deliberately or the gene deleted virus strain variant has been introduced accidentally, nucleic acid testing may fail in some animals because the amount of virus that is produced is much lower compared to the wild-type field virus. However, where good samples are available from tissue or blood, a nucleic acid test for the deleted genes of the vaccine virus can be done. After a positive test for the P72 gene, a PCR test for the gene deleted vaccine looking for the presence of DNA from MGF 360 – 505 R and CD2v can be done to determine if the problem virus is the field virus or the gene deleted vaccine virus.
Loop-mediated isothermal amplification (LAMP) offers a rapid, cheap, flexible, and extremely sensitive nucleic acid alternative that requires little specialized equipment, and seems well-favoured for mass testing such as monitoring/screening at slaughter.
Serology may be used to determine if the animals have been exposed to the ASF virus when the time course from infection to testing has been long enough that the period of viremia and presence of virus in the tissues has passed or if good samples from necropsy are not available.
There are a number of ELISA kits available to look for the presence of antibody to P 72, P 30, and other ASF antigens. Such test kits are often used to identify and typically cull groups of females that have been vaccinated deliberately or accidentally exposed to the illegal vaccine virus.
There is an antigen capture ELISA card test, but it is severely lacking in sensitivity, and its use is generally limited to those cases where a quick false negative result is desired.
On histopathologic examination there is a generalized vasculitis with infarction, hemorrhage, and thrombosis in multiple organs, particularly the lung, spleen, lymph nodes, kidneys, brain, and gut. There is massive lymphoid destruction in the lymph nodes and spleen, and vacuolation of alveolar macrophages. Necrosis and ulceration of the colonic epithelium is common (Photo 4).

The use of histopathology to verify the typical chronic lesions of the gene-deleted vaccine can be very useful. Pigs that have received those vaccines for ASF will usually have chronic-active healing and fibrosing vascular lesions including thrombi and infarcts in the gut, liver, lymphoid tissues, heart, and kidneys. The lymph nodes may have areas of hemorrhage, necrosis and lymphoid destruction and fibrosing and healing zones. Vaccinated breeding animals may have massive zones of lung necrosis and fibrosis that are often mistaken for chronic APP. The vaccine virus might not kill the pig but the pig is often unable to clear itself of the vaccine virus.
One should remember that PCR is a great tool but not infallible, and, relative to the actual farm situation, is not 100% accurate. This not to say that PCR is unreliable. Au contraire... but still, PCR results are diagnostic test results not a diagnosis. The diagnostician is an investigator and should employ all of the tools at his command. When ASF is suspected, some care in biosafety is indicated as always, and even more so. But there are several ASF look-alike diseases and generally speaking a diagnosis of the actual cause of the problem is required in addition to a negative test for ASF, which may require more observational intervention than popping out an inguinal node or exteriorizing the spleen through a keyhole incision.