There are five main types of viral hepatitis in humans designated as hepatitis A, B, C, D and E. Hepatitis E is caused by hepatitis E virus (HEV; taxonomic name Orthohepevirus A), a non-enveloped RNA virus in the Hepeviridae family. Based on WHO estimates, there are approximately 20 million HEV infections every year in people worldwide. Transmission of this virus occurs frequently via the oro-fecal route often associated with poor sanitation and contaminated drinking water. In humans, HEV is commonly associated with a mild short-term subclinical infection. Signs of acute hepatitis E may include jaundice, fatigue and nausea and often manifests as self-limiting icteric illness. Progression to severe fulminant liver failure may occur in certain high risk groups. Besides humans, HEV has also been identified in a wide range of domestic and wild animals; however, information on clinical importance of HEV in the different animal species is still very limited. HEV strains can be divided into eight different genotypes (Table 1). Genotypes 1 and 2 are restricted to humans and associated with epidemics. All other genotypes in this species have been identified in a continuously expanding range of mammalian hosts. From a public health point of view, genotypes 3, 4 and 7 are known to cross species barriers and thus have the greatest zoonotic potential. Sporadic and cluster cases of hepatitis E in humans have been linked to consumption of contaminated raw or undercooked pork , wild boar or deer products and more recently camel milk.
Table 1: Genotype classification of Hepatitis E virus (HEV) or Orthohepevirus A including host range, geographic distribution and zoonotic potential.

| Genotype | Host range | Geographic distribution | Zoonotic potential |
| 1 | Humans | Asia | |
| 2 | Humans | Mexico, Africa | |
| 3 | Humans Pigs, wild boars Rabbits Deer Mongooses Moose Goats Cows |
Global | YES |
| 4 | Humans Pigs, wild boars Deer Goats Cows |
Asia, Europe | YES |
| 5 | Wild boar | Japan | Likely |
| 6 | Wild boar | Japan | Likely |
| 7 | Camel, Humans | Middle-East | YES |
| 8 | Bactrian camels | Middle-East | No |
| Not classified to date | Moose | Sweden | No |
| Little egret | Hungary | No | |
| Kestrel | Hungary | No |
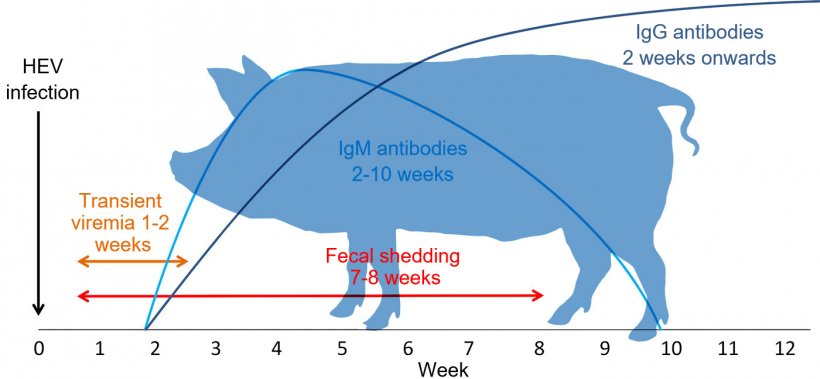
In pigs, HEV was first identified in 1997 and to date it is recognized that genotypes 3 (most commonly), 4, 5 and 6 circulate in pigs and wild boars (Table 1). HEV infection in pigs appears to be ubiquitous. The majority of pig herds in the main pig producing areas of the world are seropositive for anti-HEV antibodies. Commonly, pigs are infected subclinically, do not have any macroscopic liver lesions but may have mild multifocal lymphoplasmacytic hepatitis lesions microscopically. Pigs become infected by direct contact with feces from infected pigs or by exposure to HEV contaminated drinking water or feed. Infected pigs generally have a short viremia of 1-2 weeks of duration (Fig. 1). The time of infection to shedding of virus via feces can range from 1 to 4 weeks. Anti-IgM antibodies can be first detected by 1-3 weeks after infection and can last until 10 weeks after infection. The anti-IgG response usually becomes detectable at 1-3 weeks after infection and can persist for many months to years (Fig. 1). Most neonatal piglets have passively derived antibodies which last up to 2-3 months of age and are considered protective. Once these antibodies wane, most pigs get infected with HEV and develop an effective immune response.
Pigs and wild boars are considered important reservoirs for human infections. Transmission to humans occurs via direct contact, consumption of undercooked or raw pork or wild boar products such as sausages. Different field investigations have found that 2-11% of commercial pig livers from grocery stores located in Japan, Europe and the USA were positive for HEV RNA and the infectivity of the HEV was confirmed in animal models. Indirect contact transmission via produce exposed to HEV infected pig manure is also a possibility. HEV has been identified in field-grown strawberries in Canada and in frozen raspberries and the salad vegetable supply in Europe likely due to contamination with irrigation water. In addition, HEV genotypes 3 and 4 can also be identified frequently in seafood including oysters, flat oysters, mussels and clams which is suspected to occur via bioaccumulation from the water and viral concentration in their digestive tissues.
In recent years in China, a HEV vaccine for humans became available and appears to be efficient. While a pig HEV vaccine has been developed and tested, this product is not available commercially as the interest from the pork industry in such a product currently is limited. Humans are more likely to be exposed to HEV now as undercooked or raw pork and wild boar products are increasingly popular in certain demographic groups, pig organs are being frequently considered for use in human transplants, and pig-derived pharmaceutical products are increasingly used in human medicine. As the risk of HEV exposure appears to rise in the human population an opportunity for production and certification of HEV free meat products, especially pork, is emerging.


